December 19, 2013
The Dementia Care Economy

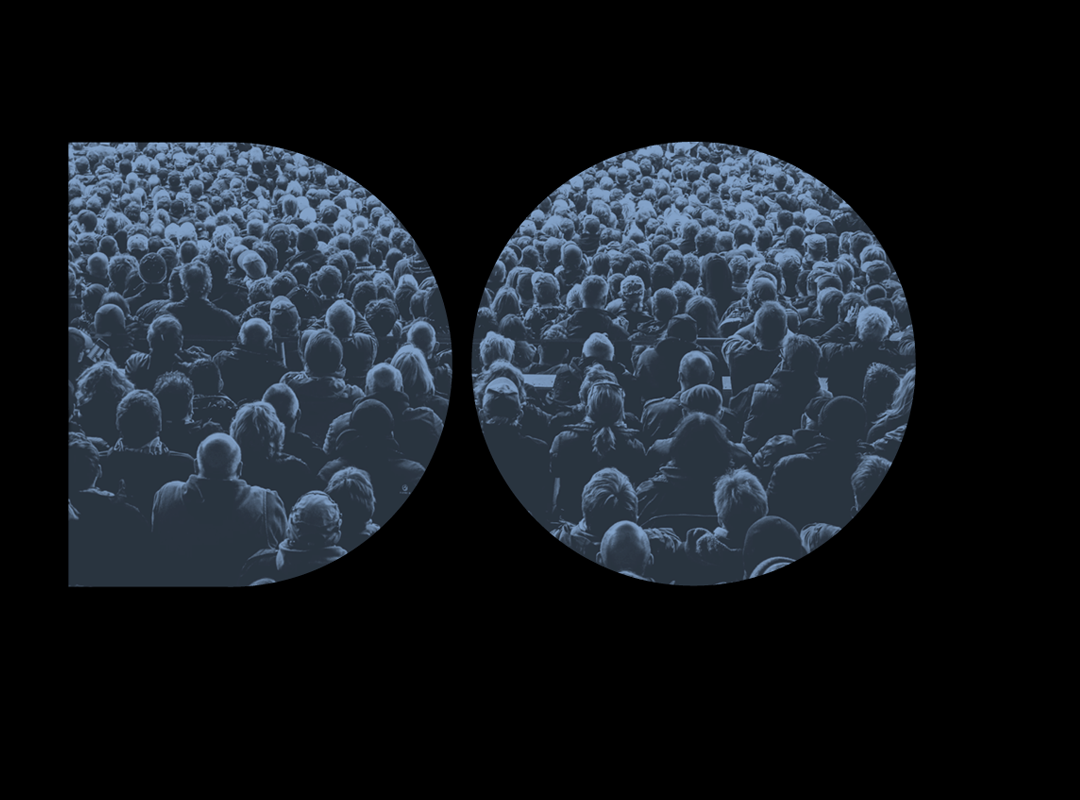
Above: the demential care ecology of Newcastle, in North East England. Illustration by Barbara Douglas
The G8 Dementia Summit made much of the fact that millions will now be spent in a race to identify a cure or a ‘disease-modifying therapy’ for dementia.
In response to that grand promise, I argued that the appropriate way for nation states to spend money on dementia would be in the ratio: 95 per cent for Care, five percent for Big Research.
I did not pluck those numbers out of thin air. They correspond to the structure of the care economy we have now.
In Wales, for example, which is not untypical of industrialised nations, unpaid carers provide at least 96 percent of annual care hours; the remaining four per cent are provided by local authorities and independent providers. Those 340,745 unpaid carers are equivalent to 11 per cent of the country’s population. In 2001, they provided at least 288.5 million hours of care; local authorities provided 11.7 million annual hours.
The social economy we yearn for already exists – but it’s unevenly distributed.
Fifty percent of older care provision in Quebec is co-operative, for example. Canada’s social co-ops have not only improved both the quality of home care for clients, but also the working conditions, wages, and professional competence of home care-givers. Coop care workers gain life-skills training. People with intellectual disabilities find employment.
In Bologna, 87 percent of elder care is cooperative. In Italy, 6,000 social co-operatives provide social services. These social co-ops employ 160,000 individuals, of whom 15,000 are disadvantaged workers.
In my conversation with Michel Bauwens last week, I learned about these facts from an important book by John Restakis, called Humanizing the Economy. It’s about a new generation of social economy organizations that pursue their goals on the basis that individuals’ contributions will be reciprocated and the benefits shared.
“Social care becomes a shared outcome between caregiver and care receiver”, Restakis explains. “This element of personal control is fundamental to the reform of social care systems, particularly for those who are most dependent—people with disabilities, the poor, and the marginalized”.
For the social co-ops in Italy and Canada, writes Restakis, their multi-stakeholder structure is a key factor in their success. Because social co-ops are controlled by a variety of stakeholders, costs are contained because they are not controlled solely by those who receive monetary benefits from the organization. Rather than operating in isolation, businesses and other agents can be linked in a networking system for mutual benefit and shared markets.
A large number and variety of stakeholders are present in the invisible care economy, too. During During Alzheimer 100: the Journey through Dementia for example, we learned that 60-70 different organisations were active in North East England helping people with dementia and their carers – often informally. (See illustration at the top of this piece).
The social economy is not an alternative to the state or central government — but it does entail a transformation of government’s role.
In Bologna, Restakis found that over 87 percent of the city’s social services are delivered via service contracts between the municipality and social co-ops. As a result, the city has experienced a dramatic growth in the number and variety of health and social services available, an improvement in the quality of care offered, and a lowering of the cost of providing these services. At the heart of this success is a unique partnership between the municipality and the broader co-op sector.
It’s not about pizzas
Health and wellbeing are not something you ‘deliver’, like a pizza. Neither are they exotic chemical compounds cooked up, at vast expense, in corporate and government labs.
This is no small shift of emphasis. The ‘delivery’ metaphor is pervasive in today’s system – as is the word ‘industry’. But those words perpetuate the myth that health is something produced by one set of people [the professionals] for another [their customers].
The beauty of the health-as-ecosystem idea is that it enables us to focus on the existing metabolic energy of people – not on the about-to-be-problematic fossil-fuel energy on which mainstream medical systems depend.
The good news is that 95% of care happens outside the medical system already; think of those three million Brits people caring for people with dementia today. The raw materials for transformation are already in place.
Observed
View all
Observed
By John Thackara
Related Posts

Equity Observer
L’Oreal Thompson Payton|Essays
‘Misogynoir is a distraction’: Moya Bailey on why Kamala Harris (or any U.S. president) is not going to save us

Equity Observer
Ellen McGirt|Essays
I’m looking for a dad in finance

She the People
Aimee Allison|Audio
She the People with Aimee Allison, a new podcast from Design Observer

Equity Observer
Kevin Bethune|Essays
Oh My, AI
Related Posts

Equity Observer
L’Oreal Thompson Payton|Essays
‘Misogynoir is a distraction’: Moya Bailey on why Kamala Harris (or any U.S. president) is not going to save us

Equity Observer
Ellen McGirt|Essays
I’m looking for a dad in finance

She the People
Aimee Allison|Audio
She the People with Aimee Allison, a new podcast from Design Observer

Equity Observer
Kevin Bethune|Essays